The quest to tackle fraud and abuse in the healthcare system requires a careful strategy. Dr. Mohamed Ghazaly, Dr. Finn Göldner and Dr. Faleh Mohammed Hussein describe steps adopted by the National Health Insurance Company.

With the introduction of mandatory health insurance schemes, governments across the Gulf region are investing in the future of their societies offering increased access, choice and quality of the care provided.
The Seha scheme managed by the National Health Insurance Company (NHIC) covers the Qatari population for a broad range of services including a schedule of benefits for dental and optical procedures. The scheme has a wide network of over 180 providers spanning both the private and public sector and is hugely popular amongst the beneficiaries.
The generous reimbursement structure compensates adequately a bundled episode of care for admitted as well as non-admitted services across the spectrum of public and private providers.

Unfortunately we know from the international experience that a small percentage of the providers in all healthcare systems are taking advantage of the system by submitting abusive and fraudulent claims. Data from the US for instance estimates the total loss due to fraud and abuse to be in the range of 8 -10 percent of healthcare spend, whilst the data from Qatar is yet to be quantified.
Types of fraud and abuse
Healthcare abuse is any activity committed either by a healthcare provider or a member that is inconsistent with sound practices (medical, financial or business) and which results in financial harm, in our case to the NHIC. In contrast to abuse, healthcare fraud is criminal in intent and a crime in all jurisdictions including the State of Qatar.
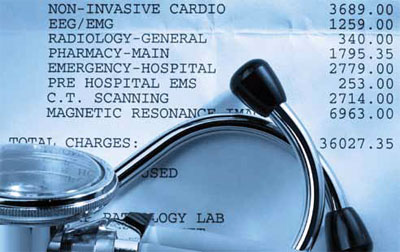
Common pattern of fraud and abuse may involve a provider misstating the type or complexity of services performed, rendering and billing for unnecessary repeat visits within a givenspecialityor unnecessary referrals across multiplespecialitiesor even billing for services not performed.
There are many other areas of fraud and abuse being initiated by members, for example identity fraud where someone lends their insurance card to someone else. However, Qatar has taken a preventive measure early on, not to create any specific insurance card for their Seha scheme, but to rely on the Qatar identification card, which uniquely and securely identifies those eligible for services.
Combating fraud
NHIC has taken a multistep approach focusing on prevention first.
A first observation after newly introducing social health insurance with standard coding and electronic submission of claims was the poor state of medical documentation. Clarifying our expectations to providers on minimum levels of medical documentation as a requirement for payment was, therefore, the first step. This was executed in collaboration with the regulator by preparing and sharing with all providers a minimum documentation standard to support the electronically coded claims details.
Next, it was important to add a much greater degree of specificity to the billing rules that support the agreed upon fee schedule. This involved extensive stakeholder discussions, conducting multiple training and re-training sessions for target provider groups and updating the reference documentation.
A continuous flow of face-to-face discussions and written communication through circulars to encourage providers to instill the right behaviours within the organisation to prevent fraud, abuse and waste by specifically avoiding over utilisation and overbilling has indeed positively contributed to the corrective action.
Still focused on process measures, we then agreed with providers on standards for conducting post-payment audits, so that providers knew what they would be audited against, but also to ensure that they could not challenge the audit findings on procedural grounds, such as being unaware of the procedures or having lack of IT solutions, as well as on a standard for recovery on how to claw back overpayments.

A simple checklist first allows us to define suspicious batches of claims for which we then stop payments while a post-payment audit is underway. As a result of patterns found, we currently are in the process of refining our provider profiling analytics to further feed the flagging of suspicious claims by enriching our powerful data mining and trend analytic tools. The recent conclusions of audits conducted have confirmed that the utilisation trends flagged by analytics feeding from our provider profiling engines have now become a powerful tool to uncover fraud, abuse and waste.

At the same time, we actively encourage members of the scheme to come forward with any suspicions of wasteful or fraudulent behavior. Interestingly, members not only revolt at the thought of somebody taking advantage of the generosity of their government but also are suffering medically in case of unnecessary and oftentimes dangerous duplication or over prescription of services. In a new “Be Our Eyes” campaign, we encourage members to take joint responsibility for combating such behavior. Similarly, we also encourage whistleblowers within the provider community to diligently and discretely notify us of any suspicious behaviour in provider utilisation and overbilling.
First successes and conclusions
After over 50 targeted audits, significant recoveries and the first cases of suspected fraud currently being prosecuted (and likely going to result in expulsion from the network plus further enforcement action towards individuals), we are seeing similarities but also differences to more established healthcare markets elsewhere in the world.

Similar to other markets that we have observed, fraud and abuse cases are not evenly distributed but cluster around known specialties (e.g., dental) and a minority of providers, who oftentimes are well known to the community beforehand for their aggressive billing practices.
Meanwhile, it is very important to take into consideration the early stage of maturation of some of the private providers who are fast changing from a cash based to a direct (and electronic) billing based model. With limited resources and little experience in best practice with regards to medical documentation and coding, providers are often overwhelmed by the new requirements of an insurance-based system, and we advise to take a constructive dialogue with providers on how to jointly improve those practices, in the interest of increasing transparency and quality of the services rendered. Bad documentation and coding in our findings oftentimes are not intentional in nature but just an expression of lack of knowledge, education and management attention.
At the same time, it is crucial to set the right tone in the beginning and signal to the young and still growing network a zero-tolerance policy for any intentional acts of defrauding the system. As such, we are looking forward to the conclusion of our first cases of full enforcement by collaborating and duly escalating to the healthcare regulator.
In the end though, international experience teaches us that fraud and abuse in healthcare will always be with us to some degree due to complex and distributed systems with one predominant payer and many providers billing for thousands of services (2) financial incentives to do so. The only lasting advantage that a payer such as the National Health Insurance Company can gain over time is a superior knowledge of the patterns of abuse through better analytics and by building a strong network culture based on trust in rewarding the right behaviour while seriously punishing the wrong behaviour.
As the National Health Insurance Company we certainly are working on both areas without deviating from our primary focus, which is the strategic implementation of the goals of the social health insurance system to ensure access, quality and affordability of the system for a sustainable future.
|